Staff shortages are a top concern for healthcare executives today, as many health systems are being pushed to review staffing ratios, shorten orientation and onboarding time, and increase overtime within an already exhausted system. With gaping holes in the workforce, the remaining staff steps in to fulfill the requirements, further straining the physical health and psychological wellness of the workforce.
The pandemic has shone a light on fractured systems and on looking at the workforce differently—and the time is now to create environments of care that support and enhance collaboration.
Research has demonstrated, especially in healthcare, that when a healthy workforce is the focus, outcomes improve. Conversely, when our workforce is shrinking and exhausted, outcomes suffer, and quality and safety, engagement, turnover, patient experience, and lengths of stay all are negatively affected.
A key solution to these challenges is a supportive organizational culture and building designs created around caring for the caregivers, which will enable them to work at the top of their licenses. It is time to turn additional energy toward reengaging staff and keeping them well. Creating a workplace environment that promotes health integration, respite and empathy takes a focused strategy, clear planning and a systematic approach. Following is advice for getting started.
An Optimized Workplace Environment
Optimizing the workplace environment and physical spaces for staff makes it easier for people to do their work and stay healthy and resilient. In addition, tailoring a staffing model for the organization that supports a future team-based wellness culture is another key to creating a supportive workplace environment. Leaders also should look at restructuring staffing models and improving programs to retain staff.
Change the workplace layout. The environment plays a pivotal role that can be retooled and used to ensure the highest outcomes for patients and staff, according to the article “Staff shortages: Environmental and organizational determinants and implications for patient satisfaction,” published April 2020 in Health Policy. Proven physical environment plans that support and improve staff retention, engagement, recruitment and overall organizational performance include:
- Creating a team collaboration work area that allows for direct visualization to patient care areas and a dedicated space for staff to work together across disciplines.
- Developing a wellness team task force to guide and prioritize the organization’s efforts.
- Providing healthy meal options for staff and discounts for healthy choices (for example, fruit, vegetables, water, salads and baked hot entrees).
- Rethinking staff break areas for active (room to stretch or share conversations) and passive (quiet area to read a book or listen to music) activities.
Staff cannot work in isolation, and with the continued reduction in workforce, changing the layout of the environment can improve care outcomes and reduce staffing requirements. Research has shown that a highly connected space can allow for improved outcomes, including an increase in patient safety.
At Henry Ford Macomb Hospital in Clinton Township, Mich., moving from several units with various total bed counts to the standard 40 beds per floor or 20 beds per zone supports efficient nurse-to-patient ratios of 1-to-4 or 1-to-5. New bed counts also create improved standardization for staffing on all units.
Tailor a staffing model to support a future team-based wellness culture. St. Dominic Hospital in Jackson, Miss., is piloting a collaborative care model using registered nurses, licensed practical nurses, certified nursing assistants and medical assistants. The goals of the redesigned staff model include:
- Transforming the nursing care model to meet ongoing RN shortages.
- Redefining how bedside patient care is provided.
- Improving effective communication across all disciplines.
A Culture of Caring
The nursing department at Henry Ford Macomb Hospital has focused on a culture-of-caring model for several years. The activities are centered around the nursing care model within Jean Watson, RN, PhD’s Theory of Human Caring (watsoncaringscience.org).
The plans for a new inpatient tower design, including the remodeling of current rooms and all community spaces, were designed with “caritas processes” in mind (examples of these processes include developing trusting, interpersonal and caring relationships; engaging in genuine teaching-learning experiences; and creating a caring-healing environment for all involved).
During planning of the project, which was completed in 2020, representatives from executive leadership and the architectural/design teams created objectives to increase efficiency, improve care experience, promote quality and safety, inspire people, maintain recognition as the premiere health system in the market and decrease costs. All objectives are intended to impact human caring.
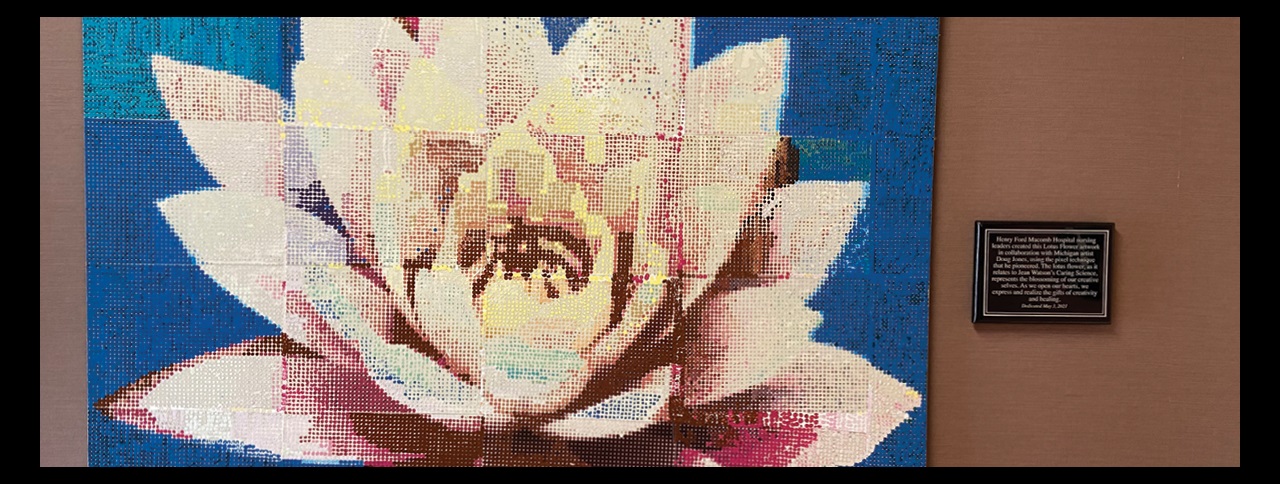
Additionally, the team partnered with Detroit-based artist Doug Jones to promote caring and healing for team members, patients and families. Initially, the artist led a group of nursing leaders in planning for and creating a work of art. Nursing leaders submitted individual pieces of pixel art that were crafted into a lotus flower.
The strategy with the pixel art technique was to bring together diverse communities in the production of a large-scale work of art. The lotus was chosen to depict the resilience of the healthcare team, patients and families. The artwork now hangs in the hallway of a medical/surgical/oncology unit.
The technological support team, inspired by the new inpatient tower design, incorporated design features that allow for the possibility to operate all rooms at any care level. Features include nursing stations located adjacent to patient rooms, in-room documentation computers, contemporary nurse call systems with transaction/data tracking, ceiling-mounted cameras with two-way audio for remote call monitoring, and e-care functions that can deliver improved patient experience through web-based tools. These technologies help ensure patients and staff are supported at all levels of care.
As health systems continue to be strained by the demands of staffing issues, considering the effectiveness of the environment that surrounds staff is vital. A curated environment that supports teamwork, reflects the organization’s culture and provides access to support allows each staff member to be fully present and able to work at their best.
Scott Kashman, FACHE, is market president, St. Dominic Health Services/CEO, St. Dominic Hospital, Jackson, Miss. (scott.kashman@fmolhs.org); Lorissa MacAllister, PhD, AIA, NCARB, is president/founder, Enviah, Grand Rapids, Mich., and an ACHE Member (Lorissa@enviah.com); and Michael J. Markel Jr., RN, FACHE, is vice president of operations/CNO, Henry Ford Macomb Hospital, Clinton Township, Mich. (MMARKEL1@hfhs.org).