Despite progress, large gaps remain in getting patients screened for colorectal cancer, one of the deadliest of all cancers if not caught early. More than 60 million patients in the United States are due for CRC screening, according to the American Cancer Society.
“Colorectal cancer is a preventable disease when caught early, yet it’s one of the least prevented forms of cancer,” says Travelle Ellis, MD, PhD, director, Health Equity Education, Strategic Partnerships and Medical Integration, Exact Sciences, Madison, Wis. “We are making progress, especially in individuals ages 50 and over. But we’re just not advancing fast enough in others.”
Closing colorectal cancer screening gaps requires a new, multifaceted approach. Following are steps health systems can take to start getting more patients screened while advancing quintuple-aim priorities such as improving patient care and addressing health equity.
Know Your Metrics
In 2021, the U.S. Preventive Services Task Force added recommending adults aged 45 to 49 (a Grade B recommendation)—in addition to adults aged 50 to 75—to get screened for colorectal cancer. Despite these updated guidelines, 80% of the younger patient population remains unscreened, according to the American Cancer Society. Keeping the newer guidelines in mind, health systems should review their screening data to make sure they’re reaching all eligible patients and adjust their outreach programs and care protocols accordingly.
Embrace Shared Decision-Making
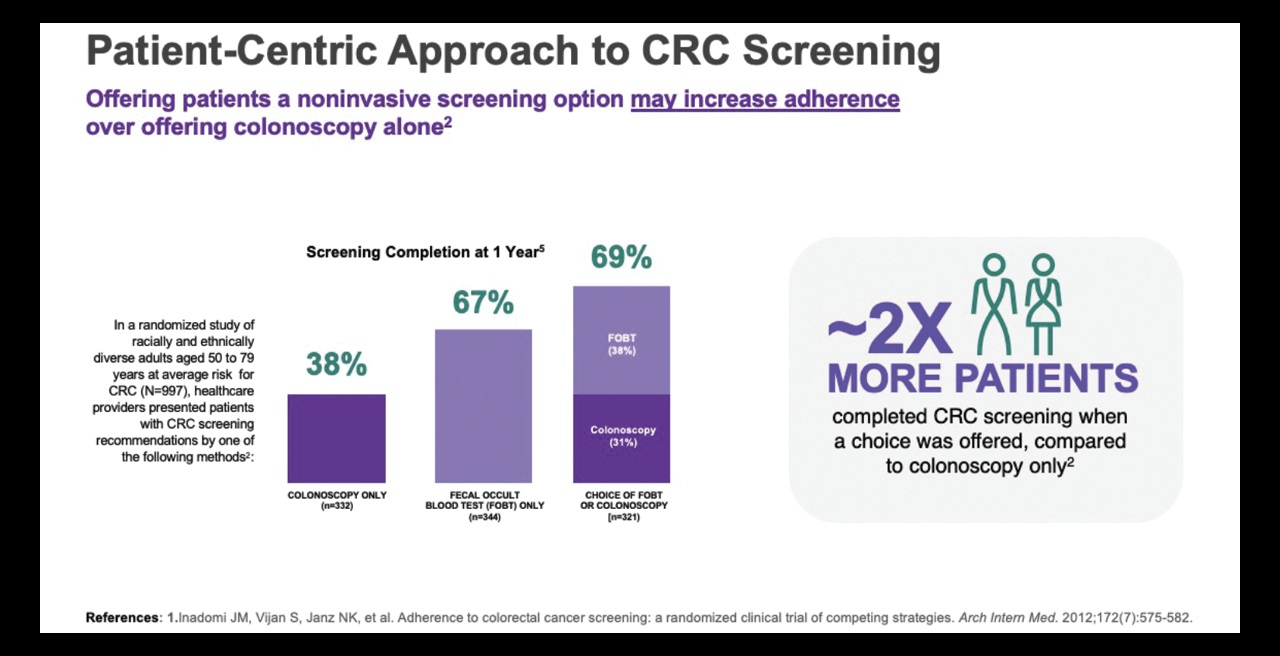
Involving patients actively in their care goes a long way toward building trust and loyalty between patients and providers while improving the overall patient experience. It also can increase cancer screening rates. Research has shown that nearly twice as many patients completed colorectal cancer screening when they were given a choice versus being offered the option of colonoscopy alone. National guidelines from the U.S. Preventive Services Task Force and the American Cancer Society recommend healthcare providers offer patients screening choices.
Choice-based, shared decision-making is at the heart of the colorectal cancer screening program at Beth Israel Lahey Health Performance Network, Wakefield, Mass., which created a Decision Aid Tool for providers to use with patients aged 45 to 75. The easy-to-read, two-page flyer (available in multiple languages at bilhpn.org/patient-resources/patient-education/) features information about colorectal cancer screening, including the risks of not getting screened and questions patients can ask their doctors.
In the pamphlet, patients can easily review information about the three main screening options: stool blood test, stool DNA test (such as Cologuard®) and colonoscopy. Two scales are also included to help patients determine their comfort level with invasive versus noninvasive tests. The Decision Aid Tool is sent to patients within 30 days prior to their provider visit, helping them feel more informed and empowered.
“It’s about getting the patient’s input and feedback and ultimately making it a two-way conversation,” says Tim Carey, project manager, Beth Israel Lahey Health Performance Network.
The shared decision-making model has increased screening rates 5% throughout the health system since it was implemented in 2022. In 2021, 68.3% of patients aged 45 to 75 had been screened. In 2022, the screening rate rose to 70.7%, and as of August 2023, the percentage stood at 73.3%. Carey expects the percentage to continue trending upward.
Collaborate With Partners
Like many organizations, Beth Israel Lahey Health experienced a lingering colonoscopy backlog due to the pandemic and workforce shortages. Collaborating with Exact Sciences to offer the noninvasive colorectal cancer screening option, Cologuard®, has increased screening capacity.
“Noninvasive tests are a key to success,” Carey says. “Getting our non-high-risk patients into noninvasive tests can help everyone get screened.”
Offering noninvasive tests can reduce structural barriers to screening, which may improve efficiencies and reduce health systems’ lab and administrative burden.
“Exact Sciences is a lab company, so we have tests and diagnostics that the hospital or health system doesn’t necessarily have to process internally,” Ellis says. Patients can have their test delivered to them and complete it at home. A package carrier then picks up the test and sends it to Exact Sciences’ lab. After the test is processed, results are sent back to the health system and provider, according to Ellis.
Collaborating with knowledgeable partners also helps organizations achieve a key quintuple-aim-related priority—health equity. Exact Sciences’ dedicated health equity team works with the company’s health system partners to provide tools and resources that support equity initiatives, such as community outreach programs that ensure vulnerable patients are included in screening efforts.
“We look at the data and work together to ensure patients aren’t being left behind, and we engage them in a language that speaks to them in a culturally competent way,” Ellis says. “These factors are important as we think about the future of healthcare because it’s a team sport, and we want to be on that team.”
Carey adds that it’s vital for health systems to learn from one another and to keep patients at the center of their efforts to increase colorectal cancer screening. “It’s about how we can all come together to improve this process, so the patient always benefits,” he says.
For more information, please contact Lindsay Reed, Director, HIT Marketing, Exact Sciences, at lereed@exactsciences.com.
References: 1. ACS. Cancer facts & figures 2023. Atlanta: American Cancer Society, 2023. Table 8. 2. United States Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States: April 1, 2020 to July 1, 2022 (NC-EST2022-AGESEX-RES). Accessed 10May2023. https://www.census.gov/data/tables/time-series/demo/popest/2020s-national-detail.html 3. Davidson KW, Barry MJ, Mangione CM, et al. Screening for colorectal cancer - US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977. 4. ACS. Colorectal cancer facts and figures 2023-2025. Atlanta: American Cancer Society; 2023 Table 5. 5. Inadomi JM, Vigan S, Janz NK, et al. Adherence to colorectal cancer screening: A randomized clinical trial of competing strategies. Arch Intern Med. 2012:172(7):575-582. 6. Wolf A, Fontham E, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250-281. 7. https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-colorectal-cancer.html
*Based on 2022 USA single year census estimates for ages 45-85 inclusive and the percentage of unscreened subjects. Does not account for variable screening rates across age ranges.