The 2020 election year will again see healthcare as a prominent issue in both national and state elections. The campaigns this fall and the initial legislative agendas from the president, Congress and state legislatures will address issues that affect consumers and systems. Efforts to control the impact of the pandemic will stimulate new legislation with increased funding for public health, improved provider financial health and telemedicine payment expansion (see May/June 2020 Healthcare Executive, Public Policy Update). Also, some elected leaders will begin to address the larger long-term issues that challenge the U.S. healthcare system.
In addition, it is likely that health disparities will receive increased attention, mostly at the state level. This is due in part to the fact that the pandemic has exposed existing disparities in healthcare access and outcomes, which have led to a disproportionate number of minorities contracting and dying from the coronavirus. Health disparities in communities of color and underserved populations are closely tied to healthcare access, family income stability, nutrition, housing, education, community engagement and neighborhood crime. Policy proposals will come from local, state and federal governments. The challenge will be developing and implementing effective coordination of these efforts to achieve needed results.
Consumer-Driven Health Policy Issues
Consumers today want their elected officials to keep the best parts of our health system while making it easier to use and less expensive. As a result, numerous consumer issues are high priorities on this year’s legislative agenda.
Drug costs. Although the pharmaceutical industry is making a valiant effort to develop vaccines and therapeutics for COVID-19, concerns will continue related to the costs of these new drugs and the overall issue of drug pricing. Legislation and administrative actions pertaining to drug costs are pending in 2020, and they will likely become part of the campaign debates. These include a major bill sponsored by House Speaker Nancy Pelosi, which would allow the federal government to negotiate drug prices for Medicare and private insurance and create a $2,000 out-of-pocket limit for drug costs for Medicare beneficiaries. The Trump administration also has advanced regulations that would allow states to import lower-cost prescription drugs from Canada, although there is pushback from some Canadian drug suppliers.
Surprise billing. Surprise billing is another issue that has received significant attention from consumers. The Centers for Medicare & Medicaid Services’ recent rule to prevent surprise billing due to COVID-19 may be a precursor to permanent legislation. A number of long-term solutions have surfaced in Congress, but competing interest groups have caused gridlock. However, many states have already implemented solutions. “As of December 2018, 25 states have laws offering some balance-billing protection to their residents, and nine of them offer comprehensive protections,” according to the Commonwealth Fund.
Preexisting conditions. The prohibition on increasing insurance premiums due to preexisting conditions was one of the most popular provisions of the Affordable Care Act. Although the Supreme Court will not act until after the 2020 election on litigation to repeal the ACA, some legislators have already introduced bills to maintain limited preexisting condition protections independent of the ACA. It is unlikely this legislation will pass in 2020, but it does provide a policy alternative.
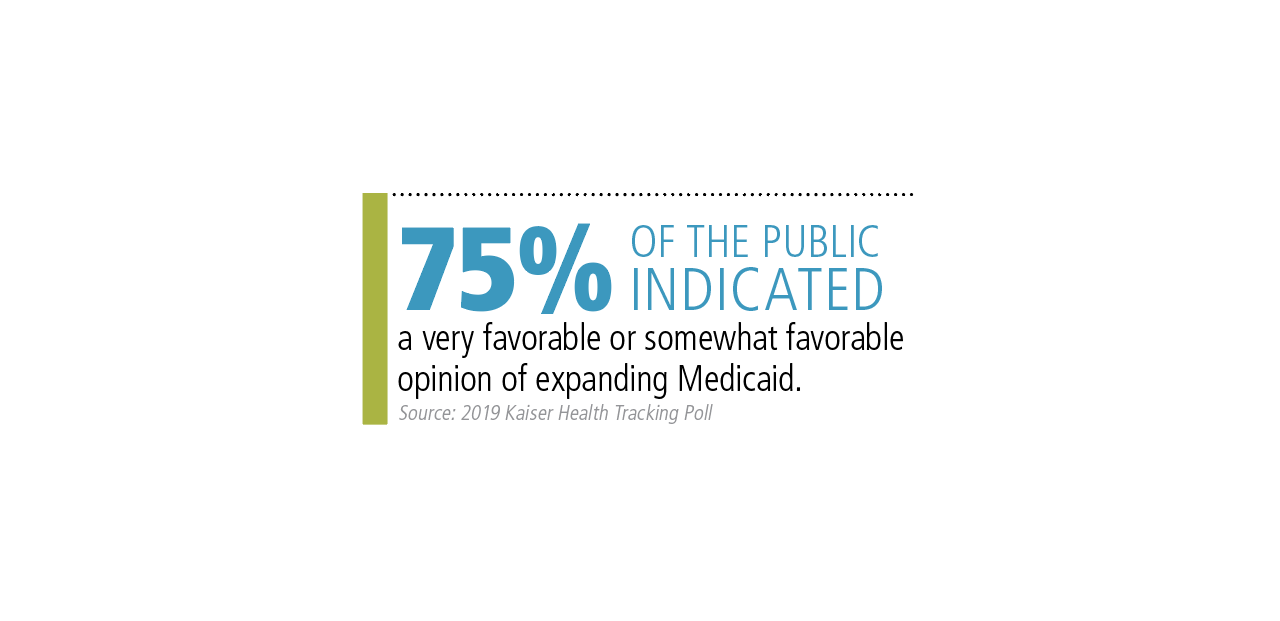
Medicaid expansion. Medicaid is a broad health policy issue that is of high concern to individuals in states that have not expanded eligibility for it, and the pandemic has further underscored the need for coverage. Medicaid is popular, according to the 2019 Kaiser Health Tracking Poll. It found that 75% of the public indicated it has a “very favorable” or “somewhat favorable” opinion of expanding Medicaid. It is likely that consumer sentiment will result in increased pressure for the 14 state legislatures that have not agreed to ACA Medicaid expansion to act on that in 2020.
Policy Improvements for System Issues
Contrary to popular belief, there are numerous health policies with bipartisan support that are able to move through Congress and be signed into law by the president. Then, there’s the federal rulemaking process, which addresses other significant health policy challenges. Although these policies may not attract significant media attention, they can have long-term effects on the fundamental structures of the U.S. healthcare system.
CMS policy initiative expansion. For example, CMS will continue to expand on existing policy initiatives such as value purchasing, price transparency and payments for improving some social determinants of health. The latter initiative is a key strategy to reducing health disparities for minority communities. Medicare is using the CHRONIC Care Act of 2018 to enable more funding of services such as telehealth, which was initially expanded during the pandemic. Many creative Medicare Advantage plans have also been using this measure to expand social determinants of health services.
State-based ACA improvements. Some state legislatures will be evaluating new policies to support the ACA, such as reimbursement pools, public option health plans and the implementation of state-based insurance exchanges.
Cost: The Long-Term Policy Issue
In February, the Trump administration released its budget request for fiscal year 2021, proposing reductions to Medicaid, the Children’s Health Insurance Program, Medicare and other healthcare programs. Although these proposals are unlikely to gain Congressional support, they illustrate the ongoing concerns about the impact of healthcare on the federal budget. The cost issue will be magnified by an increasing federal deficit due to Congressional action taken to provide funding to support the economy and employment.
However, long-term cost reductions may be feasible. A comprehensive survey of waste in the U.S. healthcare system published in the October 2019 Journal of the American Medical Association showed that a 25% reduction in U.S. healthcare costs is possible. The study identified six components of waste: nonuse of best clinical practices, failure to coordinate care, delivery of low-value care, pricing and market failures, fraud and abuse, and administrative complexity. Identifying effective policy solutions for these issues will be challenging, but some initial steps may be taken in 2020.
Although healthcare will be a prominent issue during this election cycle, actual policy enactment in 2020 is likely to be modest. However, the intensity of the debate on some issues may be a precursor for significant legislation in 2021 and beyond.
Daniel B. McLaughlin is director, Center for Innovation in the Business of Health Care, University of St. Thomas, Minneapolis, and an ACHE Faculty Associate (dbmclaughlin@stthomas.edu).
Policy Priorities in the 2020 Election Cycle
- Financial support for the healthcare system due to the pandemic
- Lowering drug costs
- Protecting against surprise billing
- Maintaining preexisting condition protection
- Expanding state Medicaid
- Enacting CMS policy initiatives (value purchasing, price transparency, social determinants of health payments)
- Improving the ACA at the state level
- Decreasing waste to lower healthcare costs